以下文章转载自:
American Journal of Neuroradiology
Presurgical Mapping with fMRI and DTI: Soon the Standard of Care?
The technique of fMRI has been around for over 30 years, and DTI for about 15 years. The first application of fMRI was by Ogawa et al, in 1990. In a rat model, this team was able to manipulate the blood oxygen level–dependent (BOLD) signal by inducing changes in deoxyhemoglobin concentrations with insulin-induced hypoglycemia and anesthetic gases. About a year later, Kwong and Belliveau published the first images of cerebral areas that responded to visual stimulation and vision-related tasks.
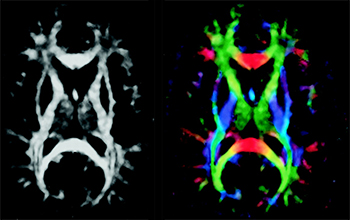
DTI was first described by Basser et al, who were experimenting on a voxel-by-voxel characterization of 3D diffusion profiles, which took into account anisotropic effects (instead of eliminating them, as in standard DWI). Tractography (or fiber tracking) was developed by applying statistical models to DTI data to obtain anatomic fiber bundle information.
Although both fMRI and DTI are now currently available in most scanners, well beyond the framework of academic institutions and research protocols, these techniques are not quite considered “standard of care.” Indeed, the processes that govern the translation of new technology into clinical practice are complex. Even more complex are the processes that lead to establishing clinical practice as standard of care, particularly at a time when established patterns of care delivery are being increasingly challenged and economic difficulties affect all aspects of society, certainly including health care.
However, some challenges, especially with fMRI, go back to basic cerebrovascular physiology. The cerebrovascular response to neuronal activation, also referred to as “functional hyperemia,” was first recognized in 1890 by Roy and Sherrington, who initially proposed a metabolic hypothesis to the phenomenon, ie, mediation via release from neurons of vasoactive agents in the extracellular space. The major role of astrocytes as key intermediaries in the neurovascular response — being interposed between blood vessels and neuronal synapses via their foot processes as modeled in the “tripartite synapse model” of the neurovascular unit — has since been recognized. Although complex, astrocyte response to changes in synaptic activity is primarily mediated by glutamate receptors through changes in intracellular Ca2+ concentration.
In fMRI, contrast is based on the BOLD effect, which reflects local shifts of deoxygenated-to-oxygenated hemoglobin ratios due to local increases in blood flow in excess of oxygen utilization following brain activity. As a result, the foundation of the fMRI BOLD signal is based on local changes in cerebral blood flow that are not linearly related to the metabolic changes inducing the flow change.
Therefore, BOLD fMRI rests on 3 major approximations: 1) the technique does not directly reflect neural activity, ie, generation and propagation of action potentials, synaptic transmission, or neurotransmitter release/uptake; 2) the changes in BOLD signal originate from that portion of the vasculature experiencing the greatest change in oxygen concentration, which occurs in the venules in the immediate vicinity of the active neurons; and 3) more importantly, fMRI signal relies on intact “neurovascular coupling,” the phenomenon that links neural activity to metabolic demand and blood flow changes.
The main reason fMRI is clinically useful most of the time is that under most circumstances neurovascular coupling remains fully intact, unaltered by confounding disorders that can interfere with this relationship. However, it has long been known that neuronal activation results in local blood flow increases that exceed local oxygen consumption, so that the oxygen utilized may constitute a small fraction of the amount delivered. Under normal conditions, the oxygen concentration in draining venules increases during neuronal activation. The original researchers who discovered this phenomenon named it “neurovascular uncoupling” or “neurovascular decoupling.” From a medical perspective, “uncoupling” or “decoupling” implies a pathologic condition, suggesting something abnormal about tissue that demonstrates this phenomenon. More recently, researchers have preferred the term “functional hyperemia” to describe the phenomenon. In fact, when there is interference with the mechanism producing functional hyperemia, the term "neurovascular uncoupling" has been re-applied, albeit with a completely opposite meaning from that originally used. Impairment in the flow response leads to neurovascular uncoupling and a reduced BOLD signal in response to neural activity, which can lead to false-negative errors in fMRI maps.
John Ulmer, reporting on a series of 50 patients, found that although accurate cortical activation could be demonstrated most of the time, various cerebral lesions could cause false negatives in fMRI results when compared with other methods of functional localization, suggesting contralateral or homotopic reorganization of function. He further suggested that pathologic mechanisms such as direct tumor infiltration, neovascularity, cerebrovascular inflammation, and hemodynamic effects from high-flow vascular lesions (ie, arteriovenous malformations and fistulas) could trigger “neurovascular uncoupling” in those patients. Neurovascular uncoupling, and other pitfalls of fMRI, are briefly discussed.
David Mikulis discusses “neurovascular uncoupling syndrome,” where lack of functional hyperemia during neuronal activation can have long-term consequences on the integrity of the tissue in the absence of acute ischemia.
Jay Pillai discusses the successful clinical application of a technique to improve the consistency of BOLD fMRI by using a breath-holding technique.
Aaron Field discusses the technique, clinical use, and some limitations of DTI and tractography, and describes patterns of alteration of white matter fiber tracts by neoplasms and other lesions.
Lastly, Wade Mueller shows that a neurosurgeon may obtain significant improvements in clinical outcomes and a drastic reduction in complication rates when working with a team that provides presurgical mapping of cerebral lesions by using fMRI and DTI (wisely, fully acknowledging their limitations) and when various team members clearly communicate using a common language.
Functional MRI and DTI are extremely useful techniques that have become increasingly available to neuroradiologists in recent years. As with any technique, these work best as parts of a whole. A good understanding of physiologic mechanisms is necessary to make us good “functional” specialists, and a good understanding of the limitations of any technique is necessary to make us better physicians.
Image modified from: Jellison BJ, Field AS, Medow J, et al. Diffusion tensor imaging of cerebral white matter: a pictorial review of physics, fiber tract anatomy, and tumor imaging patterns.
当磁共振成像(MRI)技术不停迭代创新,作为临床诊断和科学研究的工具利刃愈加锋利之时,高达 110-130 分贝的扫描噪声——相当于飞机起飞时的轰鸣声——仍旧是 MRI 扫描中难以完全克服的问题。剧烈的噪声不仅会给被试带来不适,引发焦虑情绪,更会掩盖扫描室内外的有效沟通。扫描进程中,通过耳塞、软垫等物理降噪以及佩戴耳机,被试仍可获取外部声音,但被试的实时语音则完全湮没在强噪声中,无法清晰传递给操作人员;这一方面会导致无法采集被试的语音反馈、行为指令交互等数据,另一方面也会直接妨碍某些紧急情况下的应急处理。试想,当磁共振扫描中的语音沟通不再有障碍,将会有多少新的可能!破解磁共振扫描沟通难题:美德医疗核磁语音降噪系统针对这一行业痛点,美德医疗重磅推出核磁语音降噪系统—— 一款专为MRI强噪音环境设计的磁兼容语音系统,通过技术创新,将智能硬件和自适应算法相结合,从底层解决扫描过程中的被试语音数据撷取问题。该系统的功能亮点如下:强效降噪,还原纯净语音:系统可抑制扫描噪声高达40dB,有效提取并还原被试原始语音,确保声音信号的高保真、高信噪比,为语音数据质量提供坚实保障。广谱降噪,多序列适用:不同于只针对脑功能成像序列(EPI)进行降噪的竞品,本系统具备广谱降噪能力,可根据用户需求拓展至所有磁共振机型与扫描序列,满足科学实验与临床应急的多元需求。灵活部署,即插即用:系统采用模块化设计,为独立产品形式,轻松实现扫描室内外双向清晰对讲。也可与美德脑功能视听觉刺激系统无缝对接,快速升级现有实验平台,提升研究灵活性。功能拓展,助力深度科研:支持外接USB、蓝牙、MP3等多种音源,具备双通道(降噪前后)语音同步采集功能,完整留存语音数据,支持后续精细化分析与学术输出。在认知神经科学、脑科学、心理学等研究中,清晰可靠的语音交互是实现复杂实验范式的关键。本系统有效攻克磁共振噪声干扰下的语音采集难题,为需要语音反馈的实验提供可靠技术支撑,从而显著提升数据质量与研究结果的可信度,赋能前沿科学探索。
继上半年亮相神经科学、影像技术领域学术舞台、彰显行业担当后,美德医疗在 2025 年 11 月持续以 “学术参与者”“行业协同者”“人才赋能者” 的三重身份活跃于交流前沿。短短一月内,团队跨越济南、北京、长沙、宁波四座城市,接连登陆心理学、认知科学、放射医学、磁共振影像四大领域全国性学术盛会,同步落地专业技能培训班,以深度交流促协作、以思想碰撞谋发展、以学术赋能育人才,全方位践行对多学科医疗领域进步的持续关注与积极推动。第一站:济南 | 第二十六届全国心理学学术会议(10.31-11.2)作为国内心理学领域规模最大、影响力最广的学术会议之一,第二十六届全国心理学学术会议汇聚了来自全国高校、科研院所及临床机构的数千名心理学专家学者,围绕 “心理学研究创新与社会服务价值” 展开深度研讨。美德医疗团队全程深度参与本次盛会,不仅积极融入 “科研协作生态构建”“心理学研究范式升级” 等核心分论坛,更与众多专注于脑认知、临床心理学研究的学者展开一对一交流。双方就 “跨机构研究数据协同”“心理学实验场景优化” 等行业痛点交换见解,为后续搭建心理学领域科研协作桥梁、推动研究资源高效整合奠定了良好基础。展会现场,美德医疗对心理学研究领域的关注与投入,也赢得了参会嘉宾对美德医疗品牌的高度认可。第二站:北京 | 中国认知科学学会认知与计算关系问题研讨会(11.6-7)在认知科学与计算科学深度融合的趋势下,中国认知科学学会主办的 “认知与计算关系问题研讨会” 成为领域内聚焦前沿交叉话题的核心平台。本次会议邀请了认知科学、计算机科学、神经科学等多领域专家,共同探讨 “认知机制的计算建模”“跨学科研究方法创新” 等关键议题。美德医疗创始人汤洁女士深度参与其中,重点围绕 “认知科学研究的临床转化路径”“多学科数据整合应用” 等话题分享实践洞察,探讨如何打破学科壁垒、推动认知科学研究成果更好地服务于临床需求。此次参会不仅让美德医疗更精准地把握了认知与计算交叉领域的发展方向,也为公司后续参与跨学科协作、助力认知科学临床落地积累了宝贵经验。第三站:长沙 | 中华医学会第 32 次放射学学术大会(11.13-16)作为放射医学领域的年度 “学术盛宴”,中华医学会第 32 次放射学学术大会吸引了国内外数万名放射科医师、科研人员及行业从业者,聚焦 “智能放射发展”“临床质控标准化”“放射技术临床应用升级” 三大核心方向,是推动我国放射医学领域进步的关键平台。美德医疗携近期研发新品亮相,通过展位交流、圆桌座谈等形式,倾听临床一线对放射医学领域发展的需求与期待,进一步明确了品牌 “以临床需求为导向、助力放射医学进步” 的发展方向。美德医疗对放射医学领域长期的关注与支持,也让更多行业同仁看到了品牌与领域共成长的决心。第四站: 中国体视学学会磁共振成像分会 2025 年会暨第二届诺丁汉高级磁共振成像论坛(11.21-23)会议以"磁聚·共创·振新"为主题,吸引了来自全国高校、科研院所、医疗机构及知名企业的500余位专家学者、临床医师和青年科研工作者参会,共同研讨磁共振成像领域的前沿进展与创新生态建设。通过高水平的学术交流、创新的组织形式和深度的产学研合作,有效推动了磁共振成像领域的协同创新。美德医疗深度参与交流,紧密协同体现了学术界与产业界联合发展,为构建我国磁共振成像技术创新生态体系积极贡献自己的一份力量。学术赋能不停步:美德医疗第 16 届 Task-fMRI 基础培训班在密集参与学术展会的同时,美德医疗持续深耕学术赋能,全程负责运行服务的深圳第 16 届 Task-fMRI 基础培训班同步落地。作为延续多年的品牌学术支持项目,本次培训班聚焦 Task-fMRI 技术的基础理论与实操应用,课程设置兼顾 “理论深度” 与 “实践适配性”,汇聚领域资深专家授课,为来自全国高校、科研机构的学员提供从实验设计、数据采集到结果分析的全流程指导。美德医疗团队以专业的组织服务保障培训顺利开展,助力学员快速掌握 Task-fMRI 核心技术,为行业培养兼具理论素养与实操能力的专业人才,持续为磁共振相关科研领域注入新生力量。四展连轴 + 学术赋能,初心如磐筑生态从心理学的科研协作、认知科学的跨学科融合,到放射医学的临床进步、磁共振成像的技术深耕,再到 Task-fMRI 领域的人才培育,美德医疗 11 月的学术之旅,始终以 “推动领域发展、促进行业协作、培育专业人才” 为核心。不局限于单一领域,不止步于表面参与,而是深入交流核心、倾听一线需求、分享实践见解、搭建协作桥梁、赋能行业人才,这正是医疗企业 “助力行业进步” 的责任践行。未来,美德医疗将继续以学术交流为纽带、以人才培育为支撑,持续关注多学科医疗领域动态,以更积极的姿态融入行业生态,与全球医疗同仁携手,为医疗创新发展、为更好服务患者贡献 “美德力量”!关注我们,获取更多医疗领域学术动态与品牌实践,期待与您在更多学术舞台相遇,共探医疗未来!
当深圳海风遇见成都烟火,当北京沉稳碰撞川蜀灵动,10 月 25 - 29 日,美德团队一行 47 名来自深圳、北京、成都三地的同事跨越山海,开启为期五天的川蜀团建之旅。从千年文明遗址到人间仙境,从红色初心之地到烟火市井街巷,这场兼具文化深度与团队温度的旅程,让大家在放松身心的同时,更让 “协作共赢、互帮互助” 的企业文化深深扎根。团建首站直奔三星堆遗址,青铜神树的瑰丽、纵目面具的神秘,同事们纷纷驻足惊叹。“沉睡数千年,一醒惊天下”。三星堆遗址作为中国古代文明的重要遗址之一,印证了中华文明起源的多元性。文明探源,在传承中凝聚默契,同事们第一站即为之深深触动。次日抵达都江堰,这项举世闻名的世界遗产工程,是人类和自然和谐共生的典范。站在鱼嘴分水堤上,两千多年来滋养成都平原的岷江碧水,奔流而下,大家不由得感概万千,折服于古人 “因势利导”、“道法自然” 的智慧。此次行程中,公司特意安排了汶川地震博物馆这一站,为的是让大家铭记历史,珍惜生命,关爱他人。如今站在映秀这片宁静祥和的土地上,抗震救灾的众志成城与灾后重建的涅槃重生,让不少同事湿润了眼眶。在纪念碑前,大家自发列队致敬,深刻体会到 “人心齐,泰山移” 的力量。九寨沟与黄龙的自然风光,成为心灵的治愈之旅。九寨沟的碧蓝海子、飞泻瀑布,黄龙的钙化彩池、层林尽染,让大家暂时卸下工作压力,沉浸在大自然的鬼斧神工中。同事们相互抓拍美景,分享观景心得,欢声笑语回荡山谷。登高黄龙途中,因雪天过后气温较低,路面结冰打滑容易摔跤,同事们几人一组结伴前行,相互提醒,互相照顾;行至海拔最高处,有的同事轻微高反,其他同事拿出自己的氧气瓶给同事吸氧;还有的同事下山后头疼,有热心的同事就拿出自己的药品给同事服用,这种团结互助的精神,在此次行程中得到了充分的彰显。松潘古城墙下,大家并肩漫步,聊着工作趣事与生活感悟,地域距离悄然消融,心与心愈发贴近,默契在同行中自然滋生。老板的精心安排,让川蜀烟火气成为团建的温暖注脚。正宗川味火锅宴上,红油沸腾,食材鲜香,同事们围坐畅饮,辣得酣畅,聊得尽兴。席间,老板特地为大家安排了变脸表演,演员精妙的技艺引来同事们阵阵欢呼,麻辣鲜香的火锅与非遗变脸的配搭,全员嗨翻,将氛围感和幸福感直接拉满。晚饭后,小伙伴们打卡玉林路的小酒馆,哼着赵雷的《成都》,在小酒馆门口合影留恋,温情满溢,向往已久的心情得到了无比的满足。最后一天,我们早早出发前往熊猫繁育基地,渴望亲眼见到明星“花花”,然而时间有限,我们未能一睹她的芳容,倒是拍摄到了她的其它家族成员。个个憨态可掬,或爬树,或酣睡,或仰卧着吃竹子,形态各异,可爱至极;或嬉戏打闹,或趴在树杈上睡觉,或坐成粽子状打盹背对观众,这身影,这背影,这造型,治愈了大家许久以来的焦虑和疲惫。五天的行程紧凑充实,身体虽累,内心却无比丰盈。所有同事始终服从安排、恪守时间,用行动诠释 “守时守信、互帮互助” 的团队准则。这场团建让跨地域同事从 “线上协作” 变为 “线下并肩”,让个体力量汇聚成团队合力。未来,美德医疗团队将带着这份友谊与信念,以更饱满的热情、更团结的姿态投入工作,秉持 “为善致乐,相互合作,共建和谐阳光团队” 的企业文化,携手书写公司发展新篇章!致敬每一位同心同行的 "美德人”
2025 年 10 月 22 日下午,深圳市美德医疗电子技术有限公司迎来市人大常委会教科文卫工委一行人莅临调研访谈,本次调研访谈聚焦于脑机接口产业立法相关事宜,旨在为该新兴产业的规范发展提供法治保障。调研访谈伊始,美德医疗总经理汤洁女士向市人大常委会教科文卫工委一行详细介绍了公司概况。作为国内脑功能成像领域的领航企业,美德医疗自 2004 年成立以来,始终专注于脑科学设备及医学影像配套产品的研发生产、技术培训与科研服务,为推动脑科学产业发展做出了积极贡献。汤洁女士还带领调研组参观了公司,全方位展示了美德医疗在技术研发、生产制造以及科研服务等方面的先进设施与专业团队,让调研组对公司有了更为直观、深入的了解。参观结束后,调研访谈正式开始。会议由市人大常委会教科文卫工委主任主持。市人大代表、市人大常委会教科文卫工委委员以及企业代表依次发言,围绕脑机接口产业立法展开深入交流与探讨。在发言中,美德医疗代表着重强调了脑机接口技术在医疗、康复等领域的巨大应用潜力以及当前产业发展的机遇与挑战,呼吁立法机关在保障技术创新的同时,关注伦理、安全等关键问题,为产业健康可持续发展奠定坚实基础。市科技创新局相关负责同志也对调研访谈中提出的问题作出回应,表示将积极配合立法工作,推动脑机接口产业相关政策的完善与落实。此次市人大常委会教科文卫工委到深圳市美德医疗电子技术有限公司进行调研访谈,不仅是对脑机接口产业立法工作的有力推进,更是对美德医疗在脑科学领域所取得成绩的充分认可。作为行业领军企业,美德医疗将继续秉持创新驱动、技术引领的理念,积极参与行业标准制定与立法研讨,以高质量的产品与服务助力脑机接口产业蓬勃发展,为深圳打造脑科学创新高地贡献更多力量。
8月8日-10日,由上海市生物医学工程学会主办,上海市生物医学工程学会放射医学工程专业委员会和上海交通大学医学院附属瑞金医院承办的“2025年全国磁共振学术大会、第三届医学影像产医融合创新发展研讨会”,在上海圆满召开。本次会议以“融合创新技术引领智能重塑”为主题,围绕磁共振与精准医学、人工智能赋能磁共振、磁共振对比剂与分子影像、多核磁共振代谢成像、磁共振临床应用拓展、医学影像技术临床应用转化、医学影像大模型与影像组学等热点问题,邀请到了诸多国内外著名专家学者进行主旨演讲及专题报告,精心呈现了一场兼具前沿性和实用性的学术盛宴。美德医疗作为脑科学设备及医学影像配套产品整体解决方案提供商,深耕行业21年,本次携新款“磁共振病人监护仪”参展亮相,引起热烈反响,现场大咖集聚,参观络绎不绝。继2024年率先取得NMPA注册证的磁共振病人监护仪一代,已经陆续在数十家三甲医院装机使用。本次大会展出的最新研发成果,新款“磁共振病人监护仪”适用于在患者进行MRI检查期间对成人、小儿和新生儿患者进行心电(ECG)、血氧饱和度(SpO2)、脉率(PR)、无创血压(NIBP)、二氧化碳(CO2)、体温(TEMP)监护;同时配备远程监护显示器,可以在控制室同步观测生理参数,控制血压测量操作。磁共振病人监护仪不同监护参数的选择,取决于不同的临床需求及实际使用需要,始终是特殊患者(如重症ICU患者、新生儿/小儿、麻醉镇静中的患者、进行心脏磁共振成像(CMR)、术中磁共振成像(iMRI)、磁波刀的患者等其他高风险人群)进行磁共振检查的必要监护设备。美德医疗将加速推进产品迭代,助力磁共振技术的创新发展,为安全影像保驾护航!